Nclex questions on myasthenia gravis – NCLE questions on myasthenia gravis demand a comprehensive understanding of this complex neuromuscular disorder. This article delves into the intricacies of myasthenia gravis, exploring its definition, symptoms, diagnosis, treatment, and nursing care, providing a thorough foundation for nursing professionals.
Myasthenia gravis, characterized by fluctuating muscle weakness, poses diagnostic and therapeutic challenges. This article unravels the complexities of the disease, equipping nurses with the knowledge and skills to effectively care for patients with myasthenia gravis.
Overview of Myasthenia Gravis
Myasthenia gravis is an autoimmune neuromuscular disorder characterized by weakness and fatigability of skeletal muscles. It is caused by a defect in the transmission of nerve impulses to muscles, leading to impaired muscle function.The most common symptom of myasthenia gravis is muscle weakness that worsens with activity and improves with rest.
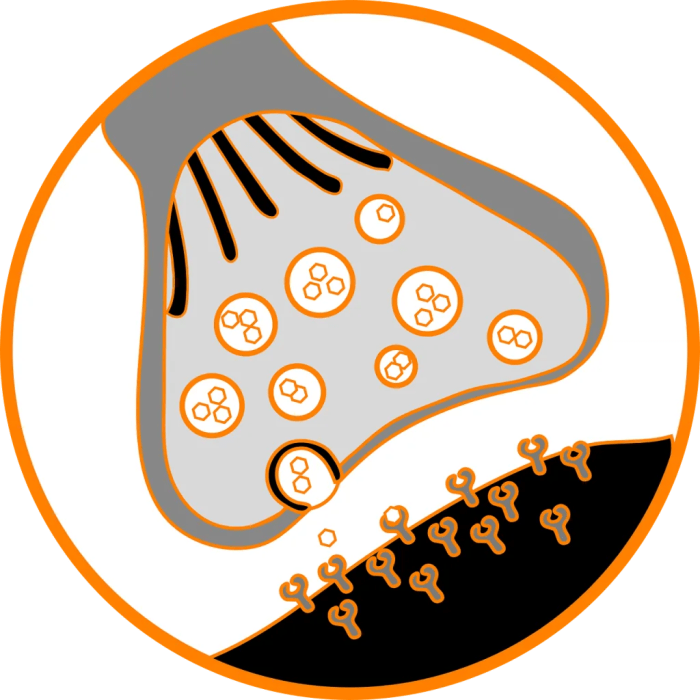
The weakness can affect any muscle group, but it is most commonly seen in the eyes, face, throat, and limbs. Other symptoms may include double vision, drooping eyelids, difficulty swallowing, slurred speech, and shortness of breath.Myasthenia gravis is caused by antibodies that attack the acetylcholine receptors on muscle cells.
Acetylcholine is a neurotransmitter that is released by nerve cells to stimulate muscle contraction. When the acetylcholine receptors are blocked by antibodies, the muscles cannot contract properly, leading to weakness and fatigue.There are different types of myasthenia gravis, depending on the distribution of muscle weakness.
The most common type is generalized myasthenia gravis, which affects muscles throughout the body. Other types include ocular myasthenia gravis, which affects only the muscles of the eyes, and bulbar myasthenia gravis, which affects the muscles of the face, throat, and neck.
Diagnosis of Myasthenia Gravis
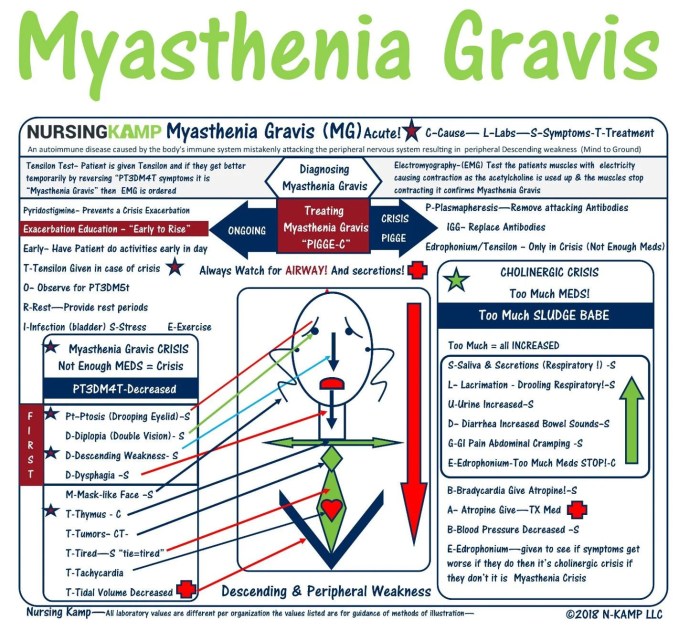
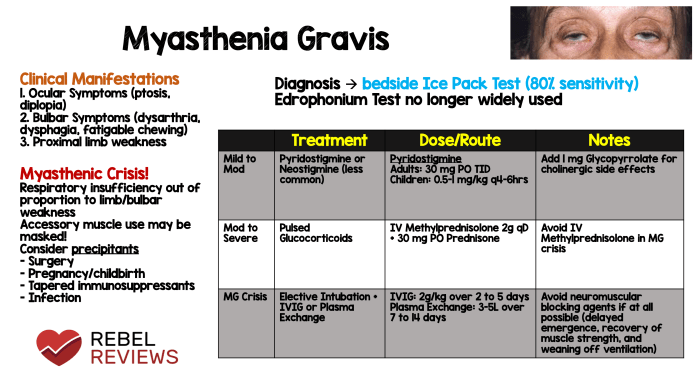
Diagnosing myasthenia gravis involves a combination of physical examination, medical history review, and specialized diagnostic tests. These tests aim to assess muscle weakness, identify the presence of antibodies against acetylcholine receptors, and rule out other conditions with similar symptoms.
Tensilon Test
The Tensilon test is a diagnostic procedure that involves administering a short-acting anticholinesterase medication called edrophonium chloride (Tensilon). This medication temporarily increases the levels of acetylcholine in the neuromuscular junction, which can improve muscle strength in individuals with myasthenia gravis.
During the test, the individual is observed for any improvement in muscle strength or other symptoms after receiving the Tensilon injection. A positive Tensilon test, characterized by a significant improvement in muscle strength, strongly suggests the presence of myasthenia gravis.
Electromyography (EMG)
Electromyography (EMG) is a diagnostic technique that involves recording the electrical activity of muscles. In myasthenia gravis, EMG can help assess the function of neuromuscular junctions and detect abnormal electrical patterns characteristic of the condition.
During an EMG, small needle electrodes are inserted into the muscles to measure electrical signals. The patterns of these signals can provide information about the strength and function of the muscles, as well as the integrity of the neuromuscular junctions.
Treatment of Myasthenia Gravis
Treatment for myasthenia gravis aims to improve muscle strength and reduce the severity of symptoms. Several treatment options are available, including medications, thymectomy, and plasmapheresis.
Medications
- Cholinesterase inhibitors, such as pyridostigmine and neostigmine, increase the levels of acetylcholine at the neuromuscular junction, improving muscle strength.
- Immunosuppressants, such as prednisone and azathioprine, suppress the immune system, reducing antibody production against acetylcholine receptors.
- Monoclonal antibodies, such as eculizumab and ravulizumab, block the complement system, which is involved in the destruction of acetylcholine receptors.
Thymectomy
Thymectomy, the surgical removal of the thymus gland, is an option for patients with thymoma or generalized myasthenia gravis. The thymus is often involved in the production of antibodies against acetylcholine receptors.
Plasmapheresis
Plasmapheresis is a procedure that removes antibodies from the blood. It is typically used as a short-term treatment for severe myasthenia gravis or during exacerbations.
Nursing Care for Patients with Myasthenia Gravis: Nclex Questions On Myasthenia Gravis
Nursing care for patients with myasthenia gravis focuses on assessing and monitoring symptoms, managing complications, and providing patient education and support.
Assessing and Monitoring Patients with Myasthenia Gravis
Nurses play a crucial role in assessing and monitoring patients with myasthenia gravis. This involves:
- Observing for signs and symptoms of myasthenia gravis, such as muscle weakness, ptosis, diplopia, and dysphagia.
- Monitoring vital signs, including respiratory rate and oxygen saturation, as respiratory muscle weakness can be life-threatening.
- Assessing the patient’s ability to perform activities of daily living, such as eating, dressing, and walking.
- Evaluating the patient’s response to treatment, including the effectiveness of medications and the need for adjustments.
Pharmacology of Medications Used in Myasthenia Gravis
Medications used to treat myasthenia gravis target either the neuromuscular junction or the immune system. The main classes of medications include anticholinesterase drugs and immunosuppressants.
Anticholinesterase drugs, such as pyridostigmine and neostigmine, increase the amount of acetylcholine available at the neuromuscular junction, thereby improving muscle strength. Immunosuppressants, such as azathioprine, mycophenolate mofetil, and cyclosporine, suppress the immune system to reduce the production of antibodies that attack the neuromuscular junction.
Table of Medications Used in Myasthenia Gravis
The following table summarizes the different medications used to treat myasthenia gravis, including their mechanism of action, dosage, and side effects:
| Medication | Mechanism of Action | Dosage | Side Effects |
|---|---|---|---|
| Pyridostigmine | Inhibits acetylcholinesterase, increasing acetylcholine levels at the neuromuscular junction | 30-120 mg every 4-6 hours | Nausea, vomiting, diarrhea, abdominal cramps, headache |
| Neostigmine | Inhibits acetylcholinesterase, increasing acetylcholine levels at the neuromuscular junction | 0.5-2 mg every 2-4 hours | Nausea, vomiting, diarrhea, abdominal cramps, headache, bradycardia |
| Azathioprine | Suppresses the immune system | 1-3 mg/kg/day | Nausea, vomiting, diarrhea, abdominal pain, hair loss, rash |
| Mycophenolate mofetil | Suppresses the immune system | 1-3 g/day | Nausea, vomiting, diarrhea, abdominal pain, rash, hair loss |
| Cyclosporine | Suppresses the immune system | 3-5 mg/kg/day | Nephrotoxicity, hypertension, hyperkalemia, hirsutism |
Patient Education and Resources
Patient education is essential for individuals with myasthenia gravis to understand their condition, manage their symptoms, and improve their quality of life. Healthcare professionals should provide clear and comprehensive information to patients and their families.
Patient Education Handout, Nclex questions on myasthenia gravis
A patient education handout can provide valuable information about myasthenia gravis, including:
- What is myasthenia gravis?
- Symptoms of myasthenia gravis
- Treatment options for myasthenia gravis
- Lifestyle modifications for individuals with myasthenia gravis
Resources for Patients and Families
In addition to providing education, healthcare professionals should also connect patients and their families with resources that can provide support and guidance, such as:
- Myasthenia Gravis Foundation of America (MGFA): https://www.myasthenia.org/
- Muscular Dystrophy Association (MDA): https://www.mda.org/
- National Institute of Neurological Disorders and Stroke (NINDS): https://www.ninds.nih.gov/
FAQ Resource
What is the primary symptom of myasthenia gravis?
Fluctuating muscle weakness, particularly in the face, eyes, and limbs.
How is myasthenia gravis diagnosed?
Through a combination of physical examination, blood tests, and electrodiagnostic studies, such as the Tensilon test and electromyography.
What is the first-line treatment for myasthenia gravis?
Anticholinesterase medications, such as pyridostigmine, to improve neuromuscular transmission.